Refractive surgery
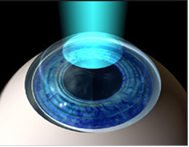
LASIK (Laser-Assisted In Situ Keratomileusis) technique is an advanced-technology refractive surgery that lasts a few minutes, is outpatient and uses topical anesthesia. The purpose is to improve the visual quality of a person having myopia, astigmatism or hyperopia.
The procedure consists in making a thin, articulated flap over the cornea allowing to shape its curvature with laser as per the patient’s needs, and removing optical anomalies. After shaping, the flap is repositioned and then affixed so it functions as a natural bandage.
Certain requirements should be met in order to perform this type of surgery: having a cornea of a certain thickness, normal and with an adequate curvature is essential. There are special circumstances where this procedure is not recommended; the surgeon will assess each particular case to determine the best treatment.
To assess whether the cornea qualifies for the procedure we conduct supplementary tests, such as pachymetry, topography and Pentacam. In case it does not qualify, other techniques can be used, such as PRK.
Photorefractive keratectomy (PRK) is another refractive procedure used to correct visual problems, such as myopia, hyperopia and astigmatism. This technique consists in making a superficial epithelial debridement and then applying laser on the cornea to shape it as intended, without the need to make the flap. Then, a therapeutic contact lens is placed, which will be subsequently removed within the first week. Because of the lack of a corneal flap, postoperative time is slightly longer and visual recovery is more slowly than with LASIK.
The final results are comparable with LASIK, but we keep this technique for particular cases where LASIK cannot be performed.
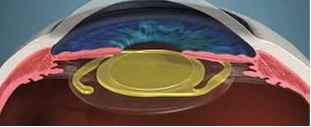
The posterior chamber phakic intraocular lens, known as Implantable Collamer Lens (ICL), is a type of lens that is placed within the eye to correct refractive faults such as myopia, hyperopia and astigmatism.
In this technique, the cornea is not modified and the crystalline is preserved. The lens is implanted behind the iris and in front of the crystalline. This technique, which enables an optimal visual quality, is ideal for persons with high refractive faults and where other laser-assisted surgeries cannot be performed in the cornea.
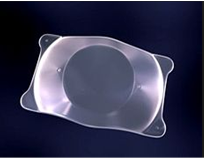
It is an outpatient procedure and uses local anesthesia. ICL lenses are made of a biocompatible material called Collamer, which is highly resistant and compatible with the eye tissue. These lenses are foldable and can be inserted by making a small incision, which reduces the need to make a larger incision in the cornea.
One advantage of ICL lenses is that they are reversible. If the eye prescription changes in the future or the lens is to be removed, an additional surgery can be conducted to extract it and replace it with another ICL lens.
Importantly, ICL lens implanting is a surgery, so there are potential risks associated with ICLs and it should be performed by an ophthalmologist specialized in anterior segment surgery. Each case is unique and the ophthalmologist will determine whether the ICL lens are appropriate as per the person’s individual characteristics.
Phacorefractive surgery combines two surgical procedures: phacoemulsification and refractive surgery. This approach is used to correct vision problems (myopia, hyperopia, astigmatism and presbyopia) in patients over 45 years old.
Phacoemulsification is used to remove the crystalline or cataract (once it starts to get cloudy). During phacoemulsification a small incision is made in the cornea and ultrasound is used to fragment and remove the crystalline by preserving the capsular bag. Once the crystalline is extracted, an intraocular lens designed to correct refractive faults is implanted, such as the multifocal intraocular lens, the extended-range lens (EDOF) or the toric lens (to correct astigmatism).
Importantly, phacorefractive surgery is a more complex procedure which combines two surgical techniques and should be performed by an ophthalmologist specialized in anterior segment and refractive surgery. Each case should be assessed individually to determine the suitability and the best treatment options.