Tests
What is it for?
It is a computerized test that helps determine objectively the eye’s vice refraction, whether myopia, hyperopia or astigmatism.
How is it performed?
It can last between 10 and 30 seconds and provides the specialist with an estimation of the patient’s visual defect.
Preparation:
No preparation required; if contact lenses are used, they must be previously removed.
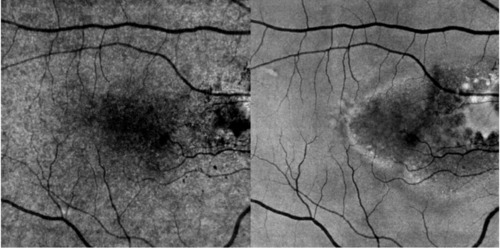
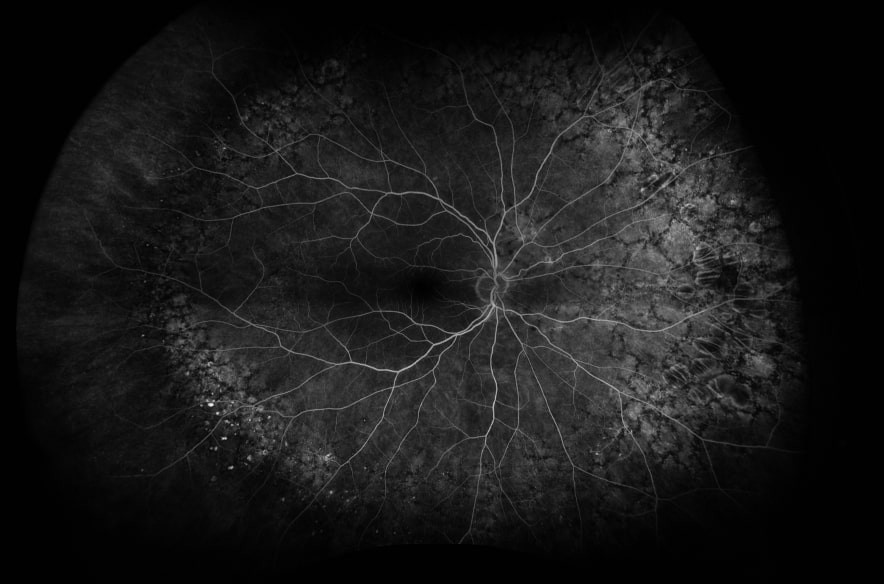
OCTA is a non-invasive technique that uses OCT technology to study the micro-circulation in the different layers of the retina and the choroid. Its advantage over conventional angiography is that it does not require pupil dilation (in most cases) and intravenous contrast injection.
It allows imaging the microvasculature of the retina and the choroid by looking at the movement of the red blood cells inside the vessels, so it does not require any contrast agent. In some cases, if there are cataracts that hinder the visualization of the retina, drops are used to expand the pupils and enhance the test results.
It is used to diagnose and follow up multiple retinal disorders such as diabetic retinopathy, age-related macular degeneration, central serus choroidopathy, vascular occlusions, macular telangiectasia and choroidal neovascular membrane of diverse causes.

An efficient solution for the workflow that joins corneal topography and tomography, the metrics of the anterior segment, the measurement of axial length and the calculation of the intraocular lens to transform the daily routines in cataracts and refractive surgery, and in cornea and glaucoma diagnosis.
What is it for?
Uses high-resolution swept-source OCT imaging to provide the most relevant tests and measurements of the anterior segment in a modular and updatable platform.
Campimetry is a medical visual test used to rule out potential visual field alterations.
What is it for?
his procedure allows assessing the patient’s visual field, detecting early alterations and diagnosing diseases of the retina, the optical nerve and the visual tract. It is essential in the diagnosis and follow-up of patients with glaucoma.
How is it performed?
It is a non-invasive fast procedure where the patient simply presses a button when they perceive the stimulus offered by the perimeter.
Preparation:
No preparation required.
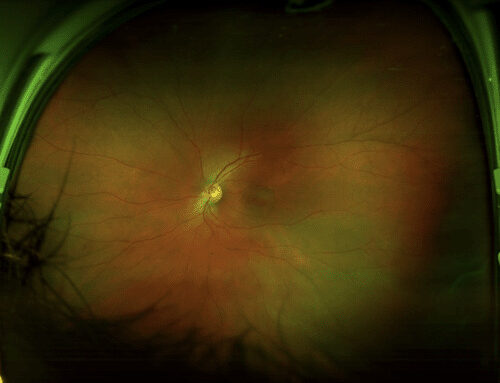
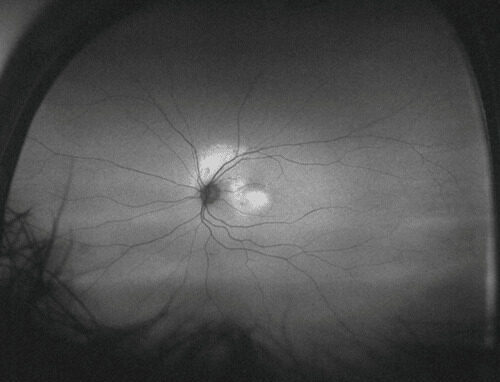
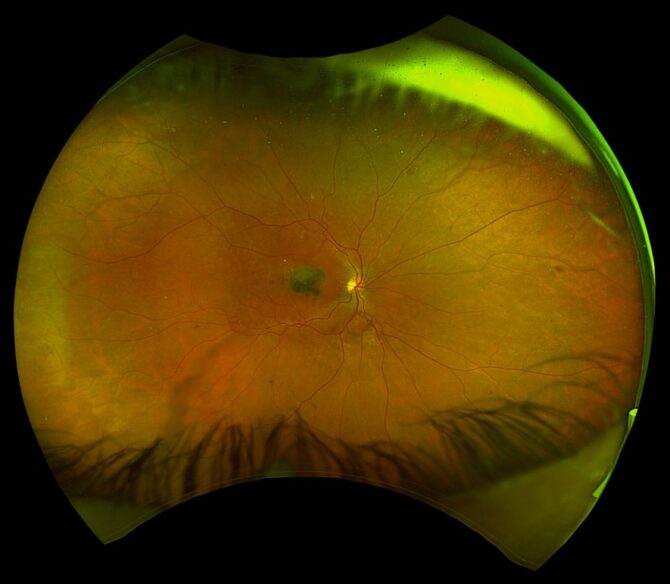
The evaluation of the back portion of the eye (retina) is performed through fundoscopy. This technique requires an experienced ophthalmologist, the patient’s cooperation and that pupils be dilated with drops (drops last half an hour to expand the pupil and the patient usually experiences blurry vision during the hours following the test, until the pupil size normalizes).
Daytona is a state-of-the-art piece of equipment that allows capturing wide-field retinal images (digital retinal imaging) in a few seconds without the need to dilate the pupil. In other words, it is a digital, fast, reliable and easy-to-perform fundoscopy.
With Daytona it is possible to diagnose and monitor retinal diseases in multiple times, such as diabetic retinopathy, diverse types of maculopathies, retinal tumors, retinal tear or detachment, and it even facilitates performing fundoscopy in children.
Digital retinal imaging can be made in color or with a filter called Autofluorescence, which allows evaluating the integrity of the retina’s epithelium. This last technique has proven extremely valuable as it provides information that traditional fundoscopy and even color retinal imaging cannot, so it has become a great tool for assessing diseases affecting the retinal pigmentary epithelium (central serus choroidopathy, age-related maculopathy, vitelliform maculopathy, etc.).
The enhancements made to Daytona software over the years now even allow evaluating retinal areas of difficult access with traditional fundoscopy. In addition, Daytona enables the ophthalmologist to explain the pathologies to their patients and to provide treatment options more easily, as they can view them directly in the photographs.
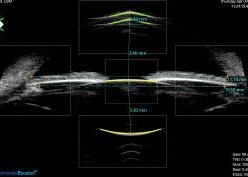
Ecosonography that allows detecting pathologies inside the patient’s ocular cavity and the orbit.
What is it for?
Used to detect corneal opacities or cataracts, retinal or vitreous detachment, vitreous or hemovitreous hemorrhage, crystalline alterations, presence of foreign bodies and ocular tumors.
How is it performed?
The patient lies down on the stretcher and closes their eyes. Soluble gel is applied on the upper eyelid and the proper high-frequency linear transducer is placed on each eyelid to examine both eyes.
Preparation:
No makeup should be used on the day of the test.
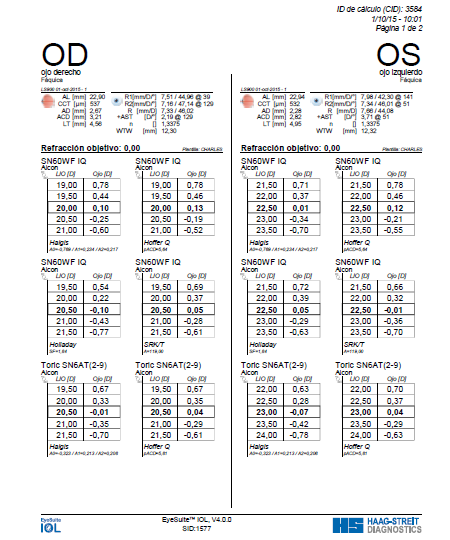
What is it for?
To estimate, by using mathematical formulas, the power of the intraocular lens to place during the cataract surgery, based on the measures of diverse ocular anatomic parameters, such as axial length, corneal curvature and depth of the anterior chamber.
How is it performed?
The patient lies down on the stretcher with their eyes closed. Soluble gel is placed on the upper eyelid and the proper transducer is placed on the eyelid. This is a non-invasive ophthalmology test that uses topical anesthesia (drops).
Preparation:
No preparation required.
It is the photographic record of the surface and the anterior segment of the eye, made with a high-resolution camera adapted to the slit lamp. Highly useful to follow up several disorders, such as pterygium and ocular nevus (mole).
It is the last technology available for testing dry eye. It consists of a corneal topographer fitted with a high-resolution camera that allows examining the tear and assessing parameters such as:
- Height of the lacrimal pathway
- Sensitivity and stability of the lacrimal film
- Thickness of the lipid layer
- Dynamics of the lacrimal film
- Record of bulbar redness
- Meibography test
What is it for?
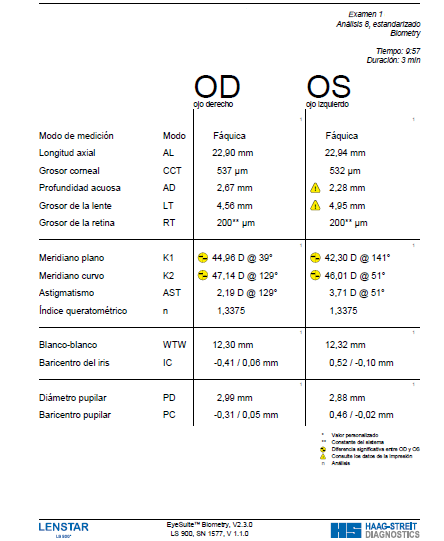
The Lenstar biometer, used as the basis for measuring OLCR (low-coherence optical reflectometry), provides several adequate means in a single measurement process.
How is it performed?
The patient fixes their vision on one single static point and all the values are rapidly obtained:
- Pachymetry
- Keratometry
- Pupil diameter
- Eccentricity of the visual axis
- White-to-white distance
- Depth of anterior chamber
- Thickness of the crystalline Axial length
- Thickness of the retina
It can determine in a single session, without contact and with great accuracy:
- The axial dimensions of the eye using 16 scans as the primary measurement
- The exact values of the different elements of the outermost portion of the eye
- The calculation of the most appropriate intraocular lens
Especially useful in eyes with high myopia, aphakic or containing silicon oil.
Preparation:
The patient has to lubricate their eyes with eyedrops for 10 days before the test (four times a day) and stop using contact lenses for the same number of days.
Confocal microperimetry is a quantitative non-invasive test whereby central vision is monitored. It does not require dilation or correction of the patient’s refraction.
It assesses the functionality and sensitivity of the macula. The test projects light stimuli over the retina and the patient hast to press a control device every time they believe they see a stimulus.
MAIA has different programs: fast mode and expert mode. Expert mode has different strategies which can be selected depending on the patient’s diagnosis.
The test allows detecting small changes in macular sensitivity or in the area of fixation.
It is a non-invasive diagnostic technique that enables to obtain optical sections of the eye with high definition, contrast and resolution. It substantially improves classic optical microscopic techniques and is especially useful in ophthalmology for the non-invasive examination of the cornea. Provides a detailed 3D examination that allows studying with greater accuracy the eye’s structures and detecting potential anomalies or diseases.
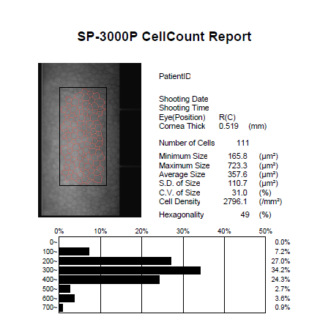
Specular microscopy is a test that determines the number, size and shape of endothelial cells by way of high-resolution images that allow examining the cells and detecting potential pathology in the corneal endothelium, such as dystrophy and corneal degeneration. It is also performed in patients undergoing cataract surgery and refractive surgery with phakic intraocular lenses.
Prior to any surgical procedure involving work inside the eye or the cornea, the cornea’s ability to keep its transparency after the procedure should be evaluated. This transparency is essential for a good vision in the operated eye and is directly dependent on the cell population of the posterior portion of the cornea (endothelium). The better the state of the endothelium is, the faster the patient’s recovery will be, and the lower the risk will be of having to undergo a corneal transplant in the short term as a secondary effect of any complication.
Preparation:
It is an easy to perform test that requires no pupil dilation and lasts nearly 5 minutes. The patient has to lubricate their eyes with eyedrops for 10 days before the test (four times a day) and stop using contact lenses for the same number of days.
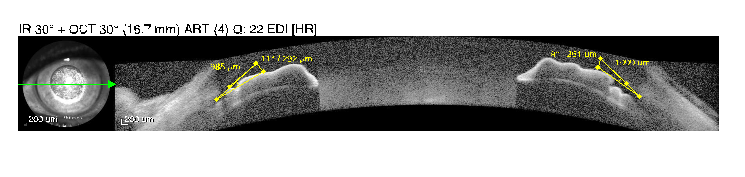
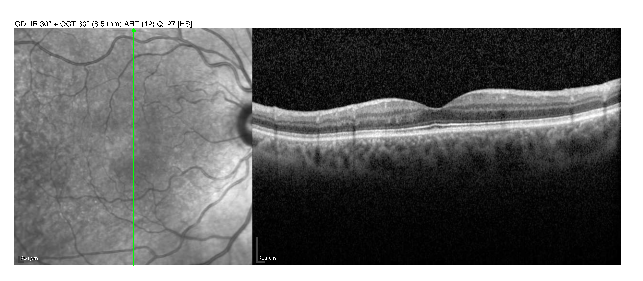
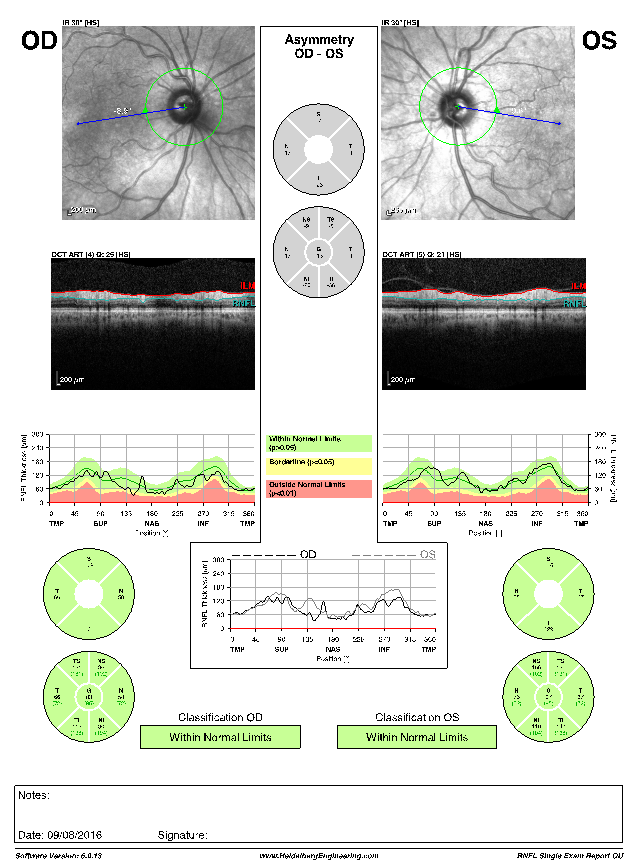
OCT is an imaging tool of great value in ophthalmology. As its name indicates, it is a tomography of the different eye tissues which allows assessing their integrity in great detail.
It can be used to examine the eye’s posterior structures, such as the retina and the optical nerve, as well as the eye’s anterior structures such as the cornea, the iris and the space between them, called anterior chamber. OCT enables diagnosis and follow-up of diverse disorders, including glaucoma (as it evaluates the optical nerve), maculopathies of diverse causes (diabetic retinopathy, age-related maculopathy or maculopathy resulting from other causes, or macular edema secondary to vascular disorders).
It is a rapid, non-invasive, high-resolution technique that requires no pupil dilation. It is currently considered an essential tool for the diagnosis and management of multiple ocular disorders.
What is it for?
Pachymetry is an easy, rapid and painless exploration that measures the corneal thickness. It has several applications, such as in supplementary exploration in glaucoma to decide a potential refractive surgery or even in the diagnosis and follow-up of certain corneal diseases.
In the case of glaucoma, it should be noted that the corneal thickness is connected to the measure of the intraocular pressure, so corneal thickness that is above or below the measure may result in biased readings in pressure measurement devices, which should be corrected.
As to refractive surgery (LASIK or PRK), pachymetry is one exploration to decide whether a person can be operated with laser to treat myopia, hyperopia or astigmatism, because during surgery a certain amount of tissue will be extracted that will directly affect the corneal thickness. Therefore, the cornea should be sufficiently thick in order to correct a specific number of diopters.
It is also used in the diagnosis of certain disorders where there is corneal slimming, as in keratoconus, or thickening, as in corneal edema.
How is it performed?
The ultrasound wave is reflected by the cornea’s posterior part (as an echo) and returns to the transducer, which in turn converts the wave into electricity, and is sent back to the microprocessor, which calculates the time the wave lasts since it is issued until it is captured. The measured time is translated into distance, which determines the thickness of the cornea (in microns, 1 cm = 100 microns).
Preparation:
El paciente debe suspender los lentes de contacto 10 días antes del turno.
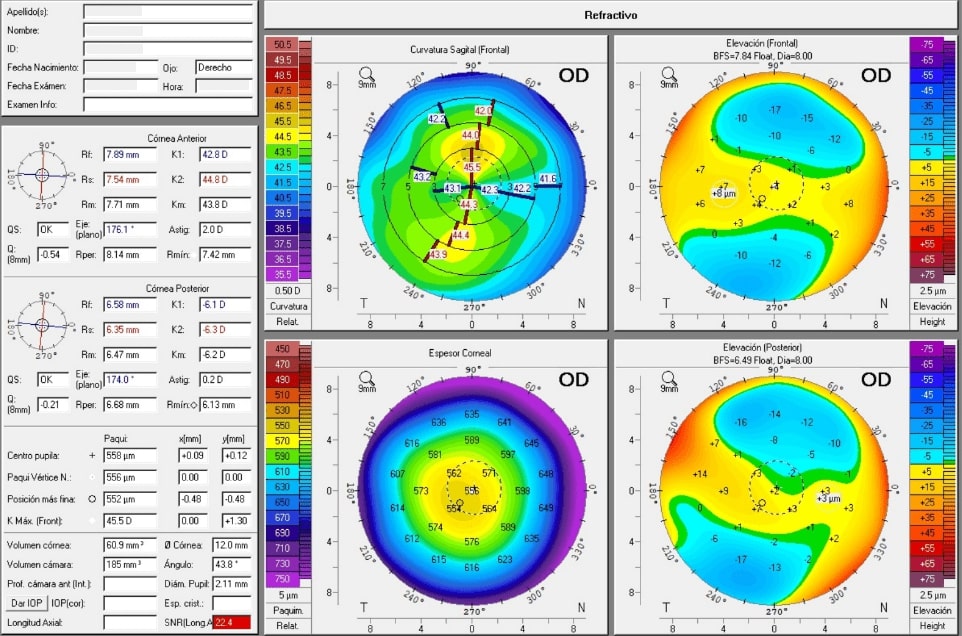
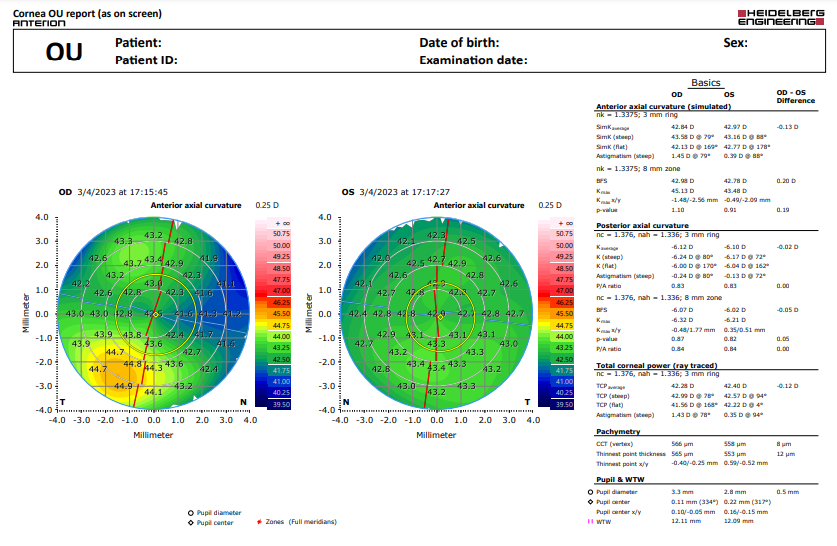
The topographic system called Oculus Pentacam, based on Scheimpflug technology, is a real advancement in terms of studying the corneal thickness supplemented by corneal topography (anterior and posterior part) information.
It allows studying the cornea rapidly, comfortably and with no contact. Pentacam has automatic security systems that make it highly reliable and repeatable, even in corneas with stromal diffuse opacity, leucomas or irregularities.
It uses a Scheimpflug camera and a processor that allows obtaining up to 50 images in less than 2 seconds and creating 2D and 3D images of the eye’s anterior segment structures.
It provides immediate information on the depth and volume of the anterior chamber, pupil diameter, crystalline density, corneal aberration measurements, topography, analysis of corneal ectasia, keratoconus and calculation of intraocular lenses (monofocal, monofocal toric and multifocal), in addition to patients who have
undergone refractive surgery.

RFG is a test that allows studying the eye’s posterior portion (the retina) and its circulation/vasculature by way of intravenous contrast injection (fluorescein). Thus, the test requires a prior allergy test for fluorescein. This test can be done in the Clinic.
RFG begins by placing drops to dilate the pupils, which last approximately 15 minutes to take effect. Then, fluorescein is injected into an arm’s vein. The colorant takes 10-15 minutes to travel throughout the body until it finally reaches the eye’s blood vessels, making them bright upon being filled with the colorant. As the colorant travels through the retina, a high-resolution special camera takes pictures of it. The test takes approximately 20-30 minutes.
Currently, RFG allows taking wide-field images, i.e., it covers areas of the peripheral retina that are difficult to evaluate. Additionally, it enables the diagnosis and follow-up of diverse retinal disorders, including diabetic retinopathy, macular edema of diverse causes, artery/vein occlusions of the retina, epiretinal membrane, retinal tumors such as melanoma, etc. It also serves as a guide to perform laser-assisted treatment of the retina.
This test is mainly used to determine if the patient qualifies for RFG (retinofluoresceinography), a test that examines the eye’s posterior portion through the injection of a contrast called fluorescein.
It is a procedure to indirectly measure intraocular pressure (IOP) using a tonometer. Intraocular pressure is the pressure exerted by the fluids contained in the eye globe’s interior (vitreous humor and aqueous humor) over the eye’s firm structures.
What is it for?
It is a simple and safe technique to detect an increase in pressure readings inside the eye globe and to conduct a follow-up thereof.
A sustained or very sudden increase in intraocular pressure readings can lead to irreversible damages to the optical nerve, which may translate into partial or complete vision loss. Tonometry is a test used to help in the diagnosis and follow-up of eye diseases, such as glaucoma.
Intraocular pressure and blood pressure readings are independent of one another.
How is it performed?
Applanation, contact or Goldmann’s tonometry consists in the indirect measurement of intraocular pressure using a tonometer placed in a slit lamp. It is the most common method employed. In applanation tonometry, the specialist places an anesthetic drop in each eye and uses fluorescein colorant during the test.
No-contact or air-assisted tonometry uses a jet of air to flatten the cornea and thus measure the intraocular pressure.
Preparation:
The patient should not be wearing contact lenses, as this test requires the use of fluorescein, which may damage them.
This test makes a full representation of the whole corneal surface, measuring variations in curvature.
The information provided by topography is decisive in the following cases:
- Measurement to implant intraocular lenses in patients with cataracts
- Better adjustment to contact lenses
- Diagnosis and follow-up of corneal degenerative disorders
- Evaluation of potential patients for refractive surgery (myopia, hyperopia or astigmatism)
How is it performed?
Corneal topography must be performed over a cornea “at rest”; therefore, it is essential that no contact lenses be used some days prior to the test and that the cornea be largely lubricated.
Preparation:
The patient has to lubricate their eyes with eyedrops for 10 days before the test (four times a day). In addition, they should not use contact lenses during the days before the test: for soft contact lenses, a minimum of 7 days, and for flexible lenses, at least 15-20 days.
It is a supplementary diagnostic imaging method designed to examine the eye’s anterior segment structures both qualitatively and quantitatively, using ultrasound (echography) to capture high-resolution images.
Like every echography, it requires an aqueous medium so that ultrasound may go through the eye’s anterior structures and generate images.
What is indicated for?
Glaucoma, trauma, strabismus, tumors, prior to or after eye surgeries, medium opacity that prevents from looking into the eye’s anterior segment, etc.
Who performs it?
An ophthalmology physician trained in eye echography.
Does it require prior preparation?
No. The patient only needs to avoid using eye makeup and creams in the region surrounding the eyes on the day of the test. If possible, patient should bring a hand towel.
How is UBM performed?
The patient lies down on the stretcher and is given anesthesia drops to avoid discomfort during the test. Then, a plastic or silicone cup (immersion cup) filled with liquid is placed over the eye surface and lastly an ultrasound probe (UBM), which remains suspended in the liquid without touching the eye. The patient must cooperate by following some indications. It is a painless, rapid and little invasive test.
Must the patient be accompanied?
No accompanying person is required.
Can I carry out normal activities after the test?
After the test, the patient can perform their normal activities, even driving.